Frozen Shoulder
What is a frozen shoulder?
A frozen shoulder (sometimes called ‘adhesive capsulitis’) refers to the inflammation and thickening of the capsule (lining) of the shoulder joint that leads to significant stiffness and loss of movement of the shoulder. It is a self-‐limiting condition that most commonly affects those over the age of 50 years. It affects up to 5% of the population but is more common in diabetics (20%) and is associated with other medical conditions including thyroid, heart and lung disease, connective tissue diseases and neurological conditions that affect movement of the upper limb. Approximately 50% of those who suffer a frozen shoulder may also develop a frozen shoulder on the opposite side.
Types of frozen shoulder
A frozen shoulder may be classified as either a ‘primary’ or ‘secondary’. A ‘primary’ frozen shoulder has no identifiable cause with the onset of symptoms being very gradual and progressive, whereas a ‘secondary’ frozen shoulder may develop after trauma to the shoulder, or following periods of immobilisation of the arm such as after surgery to the shoulder.
Causes of frozen shoulder
Studies that have attempted to identify the pathology in frozen shoulder have found inflammatory changes and thickening in the shoulder joint capsule and associated ligaments, however, the reason for the development of this pathology remains unknown. In the case of primary frozen shoulder, no causative factor can be identified, however some medical conditions (described above) have been associated with the development of a frozen shoulder. A secondary frozen shoulder may develop following post-‐surgical immobilisation of the arm, or after trauma to the shoulder, and even relatively minor trauma such as a bump or reaching movement may be sufficient to initiate the frozen shoulder process. Again, why this happens is unclear.
Symptoms of frozen shoulder
Regardless of whether the condition is primary or secondary, all frozen shoulders follow a very predictable course. They are typically painful in the early stage and later develop a generalised loss of shoulder movement particularly affecting the movement of shoulder external rotation.
Symptoms of a ‘primary’ frozen shoulder begin gradually and may progress so slowly that patients often do not seek medical advice until the symptoms have become severe and debilitating. Symptoms from a ‘secondary’ frozen shoulder tend to begin soon after the trauma or surgery when it becomes evident that the movement of the shoulder is not returning as quickly as would be expected.
Stages of frozen shoulder
Frozen shoulders typically progress through three overlapping stages:
Stage I: Painful phase (lasting 3 – 9 months)
In this phase there is gradual onset of pain that can progressively worsen to become severe and disabling including disruption to sleep. Many patients do not seek help in this phase as they believe the pain will settle with self-‐management. Usually the pain progresses to the point where medical advice is sought. This phase can last from approximately 3 to 9 months. In the case of secondary frozen shoulder there is often more rapid progression through this phase.
Stage II: Frozen phase (lasting 4-‐12 months)
In this phase, the pain gradually reduces, however there is progressive loss of shoulder movement, particularly in elevation (overhead) and external rotation movements. There may still be some pain when the shoulder is pushed to it limit of motion. Because of the long term nature of these conditions, there is also associated loss of muscle tone and strength around the shoulder. All these factors result in limitation in shoulder function. This phase can last approximately 4 to 12 months, often with faster resolution in the case of secondary frozen shoulder.
Stage III: “Thawing” phase (lasting 12 – 42 months)
In this phase, there is gradual return of shoulder mobility and function. The pain has usually all but disappeared and the stiffness in the shoulder gradually reduces. In the majority of cases almost full movement of the shoulder will return over the next 1 to 4 years.
Investigations
In many cases investigations may not be required, however a plain x-‐ray is the most useful investigation to help differentiate a frozen shoulder from other joint pathology including arthritis and a posterior dislocation. Ultrasound scans are not generally useful as they often report incidental findings, most commonly involving the tendons of the rotator cuff and fluid around the biceps tendon sheath, that are not related to the symptoms of frozen shoulder and may result in unnecessary investigations and treatment interventions that are of little or no benefit.
Treatment options
1. Do nothing
In many cases, frozen shoulders will resolve over time without the need for any medical intervention.
2. Injection
In the early stages when the pain is severe, there is good medical evidence that an injection of local anaesthetic and corticosteroid (anti-inflammatory) into the shoulder joint may be beneficial in reducing the pain. In cases of severe pain, several injections may be necessary. These procedures can be performed in your doctors’/GP’s office, or can be performed with the aid of x-‐ray (fluoroscopic) guidance at a radiology clinic.2. Injection
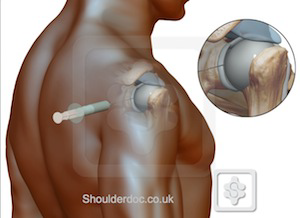
In the early stages when the pain is severe, there is good medical evidence that an injection of local anaesthetic and corticosteroid (anti-inflammatory) into the shoulder joint may be beneficial in reducing the pain. In cases of severe pain, several injections may be necessary. These procedures can be performed in your doctors’/GP’s office, or can be performed with the aid of x-‐ray (fluoroscopic) guidance at a radiology clinic.
5. Surgical (Arthroscopic) release
In resistant cases, surgical release of the shoulder joint capsule can be performed. This is keyhole (arthroscopic) surgery in which a radio-frequency probe is used to release the tight structures in the shoulder joint. The use of the arthroscope also allows the surgeon to look around the shoulder and identify any other relevant findings. Early and ongoing mobility exercises are important after this type of surgery to maintain the increased range of movement that are achieved after this procedure. There is a good success rate with this type of surgery in terms of pain, and restoration of movement.
3. Physiotherapy
In Stage III (thawing phase), physiotherapy can be of benefit to assist in stretching the tight shoulder capsular and muscle tissues, and in strengthening the muscles around the shoulder girdle to assist in the return of shoulder function. In the early stages (Stages I and II) the shoulder is often too painful to tolerate physiotherapy treatment. You do not need a medical referral to see a physiotherapist for this treatment.
4. Manipulation under anaesthetic
In cases where adequate return of shoulder movement is not occurring after an appropriate timeframe despite physiotherapy, stretching and mobilisation of the shoulder, a ‘manipulation’ of the shoulder under anaesthesia (MUA) may be recommended. This involves a period of brief general anaesthesia during which the shoulder is forcibly stretched and manipulated through its full range of movement, and a corticosteroid (anti-‐inflammatory) and local anaesthetic injection are performed for pain relief. Immediately after this procedure it is important that shoulder range of movement is maintained by the patient and/or physiotherapy treatment. Best results from a MUA are usually achieved in primary frozen shoulders when there is no longer any night pain, and stiffness is at its maximum.
For more information:
Frozen shoulder: http://shoulderdoc.co.uk/articletile.asp?article=55§ion=16&tile=1
Frozen shoulder video: http://www.shoulderdoc.co.uk/article.asp?article=1430§ion=16
Exercises: http://www.shoulderdoc.co.uk/article.asp?article=539§ion=16
Further reading:
“Frozen Shoulder” (research article) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1315655/